Letter from the Chair and Executive Sponsor
Like so many organizations, the Texas Collaborative for Healthy Mothers and Babies has been engaged in a conversation about how to stay true to our commitments while adapting to the realities of a health care system that has had to shift priorities in ways we couldn’t have anticipated even two months ago.
Dear Friends and Colleagues,
Our thoughts are with you and your families as you do your best to weather the COVID-19 crisis.
Like so many organizations, the Texas Collaborative for Healthy Mothers and Babies has been engaged in a conversation about how to stay true to our commitments while adapting to the realities of a health care system that has had to shift priorities in ways we couldn’t have anticipated even two months ago.
In light of this new reality, we will continue with our current quality improvement programs, but will shift deadlines, expectations, and metrics as needed. The leadership and committees will continue to meet, but will do so remotely and in some cases less often. We will continue to communicate about our initiatives through our newsletter and on social media, but will do so less frequently than before. We will also post perinatal-specific resources on dealing with COVID-19 on our website.
Paid staff at UT System will continue to dedicate their time to TCHMB as before, but much of the clinical leadership on the committees and in the hospitals and clinics may not be able to dedicate as much time as they were prior. And we will all continue to adapt as the situation changes.
Stay safe, and please reach out with questions and suggestions.
Sincerely,
Michael E. Speer, MD
Chair, Texas Collaborative for Healthy Mothers and Babies
David Lakey, MD
Vice Chancellor for Health Affairs and Chief Medical Officer, The University of Texas System
TCHMB Wins 2nd Place in National Improvement Video Challenge
The TCHMB-produced video, “MEWS: A Simple Alogorithm for Reducing Maternal Mortality and Morbidity, has been awarded second place in the Council on Patient Safety in Women’s Health Care’s National Improvement Video Challenge.
The TCHMB-produced video, “MEWS: A Simple Alogorithm for Reducing Maternal Mortality and Morbidity, has been awarded second place in the Council on Patient Safety in Women’s Health Care’s National Improvement Video Challenge.
Diabetes Screening and Treatment Available for Healthy Texas Women Clients
To learn more about which medications are covered, healthcare providers can access the HTW specific formulary at txvendordrug.com/resources/downloads.
Healthy Texas Women is a program dedicated to offering women’s health and family planning at no cost to eligible women in Texas. Since July 1, 2016, the HTW program has provided coverage for screening and treatment of hypertension, diabetes and high cholesterol.
In the most recent Maternal Mortality and Morbidity Task Force and Department of State Health Services Joint Biennial Report, chronic health diseases such as pre-pregnancy obesity, diabetes and hypertension were all associated with an increased risk for maternal death. The Centers for Disease Control and Prevention reports that almost 25 percent of people with diabetes and 20 percent of people with hypertension are undiagnosed.
By increasing access to vital health services and treating underlying medical conditions, women’s health and pregnancy related outcomes can improve in Texas.
Several commonly prescribed medications used to treat these conditions are available on the current HTW drug formulary. Clients approved for HTW can get these medications at any Medicaid participating pharmacy with their program identification card.
To learn more about which medications are covered, healthcare providers can access the HTW specific formulary at txvendordrug.com/resources/downloads. Participating HTW providers can access information regarding policies, billing guidelines and toolkits at healthytexaswomen.org/provider-resources.
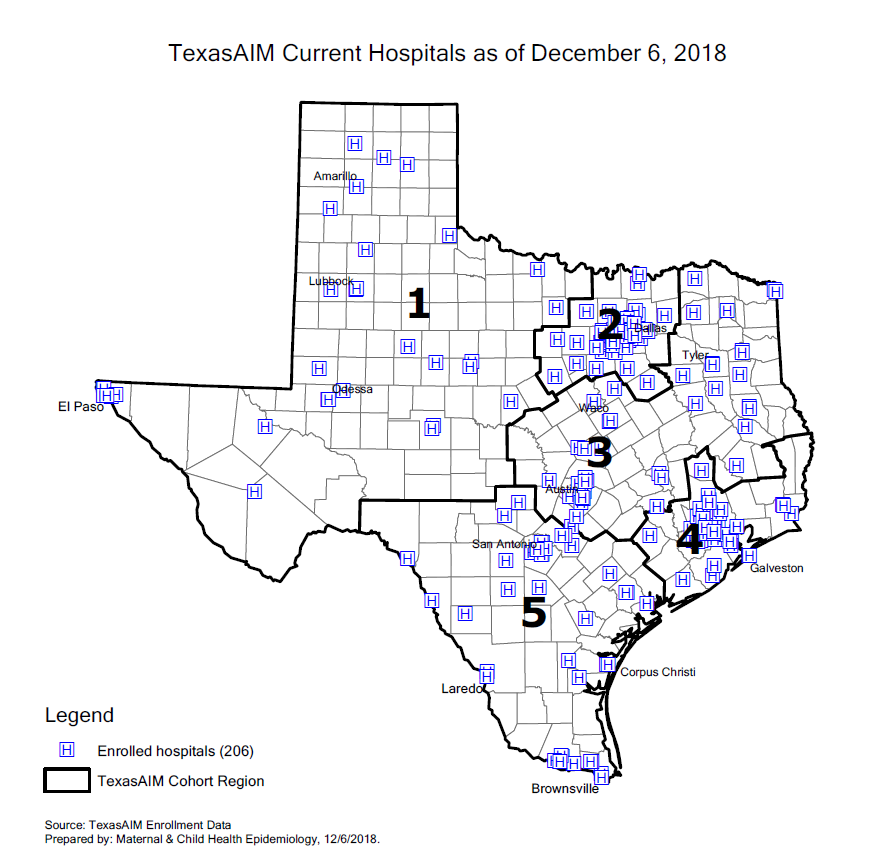
TexasAIM by the Numbers: 206 Hospitals and Counting
As of December 2018, 206 (92%) of Texas’ birthing hospitals are participating in TexasAIM. Of those, 167 are designated “TexasAIM Plus” hospitals, and the other 39 are “TexasAIM Basic” hospitals.
In our last issue, we spoke to Dr. Manda Hall, Associate Commissioner for Community Health Improvement at the Texas Department of State Health Services, about TexasAIM, a new initiative focused on reducing maternal mortality and morbidity in Texas. The initiative, which is being implemented by DSHS in partnership with the Alliance for Innovation on Maternal Health (AIM) and the Texas Hospital Association (THA), will help hospitals and clinics in Texas carry out maternal safety projects.
TexasAIM is launching with an Obstetric Hemorrhage Bundle. The initiative will then focus on the Obstetric Care for Women with Opioid Use Disorder Bundle and Severe Hypertension in Pregnancy Bundle.
As of December 2018, 206 birthing hospitals are participating in TexasAIM. That is 92% of all birthing hospitals in Texas.
As of December 2018, 206 (92%) of Texas’ birthing hospitals are participating in TexasAIM. Of those, 167 are designated “TexasAIM Plus” hospitals, and the other 39 are “TexasAIM Basic” hospitals.
Hospital Enrollment
TexasAIM Basic Hospitals: 39
TexasAIM Plus Hospitals: 167
Total TexasAIM Hospitals: 206
TexasAIM Hospital Cohorts
The AIM Plus hospitals are being divided into five cohorts, by geography, with 20-30 hospitals in each cohort. Each hospital will receive in-person learning sessions from DSHS. They will do an intake assessment, implement the QI bundles, and track and share process and outcome data over time. The hospitals in each cohort are also working together as part of learning collaboratives.
Cohort 1: 32 (16% of enrolled hospitals)
91% of participating hospitals are Plus
76% of hospitals in the region are in AIM
Cohort 2: 47 (23% of enrolled hospitals)
89% of participating hospitals are Plus
98% of hospitals in the region are in AIM
Cohort 3: 40 (20% of enrolled hospitals)
65% of participating hospitals are Plus
95% of hospitals in the region are in AIM
Cohort 4: 44 (21% of enrolled hospitals)
84% of participating hospitals are Plus
96% of hospitals in the region are in AIM
Cohort 5: 42 (20% of enrolled hospitals)
79% of participating hospitals are Plus
91% of hospitals in the region are in AIM
Geographic Area
Rural Hospitals: 74% of Rural Texas Hospitals are enrolled in TexasAIM (17 Basic, 28 Plus)
Urban Hospitals: 98% of Urban Texas Hospitals are enrolled in TexasAIM (21 Basic, 139 Plus)
AIM Data Center Portal
Registered Users in Portal: 402
Hospitals Active in Portal: 191 (93% of enrolled hospitals)
Hospitals with Structure Measures Entered: 176 (86% of enrolled hospitals)
Hospitals with Process Measures Entered: 160 (78% of enrolled hospitals)
Remembering James A. Cooley
James A. Cooley, a healthcare researcher and analyst in the Medical and Social Services division at the Health and Human Services Commission, died Nov. 11, 2017.
James A. Cooley, a healthcare researcher and analyst in the Medical and Social Services division at the Health and Human Services Commission, died Nov. 11, 2017. In his ten years at HHSC, he worked on several initiatives, including the Medicaid/CHIP super-utilizers program, but his work in improving the quality of health for Texans stretched beyond that. As a chief legislative staff member for the House Committee on Public Health and the Select Committee on State Health Care Expenditures, he worked on furthering health information technology, including helping to establish the Texas Health Services Authority.
In a post on the Texas Health and Human Services web site, Quality and Program Improvement Director Matthew Ferrara described Cooley as a sunny personality, good-natured and with formidable intellect and keen insight. Ferrara said Cooley’s contributions to healthcare and advancing health were numerous.
Neonatal Subcommittee Update
The goal of the initiative, and its associated learning collaborative, is to increase the number of very low birth weight infants that will receive human milk, preferably their mother’s milk, as their primary source of nutrition to assist with their immune and gastrointestinal tract development. More specifically, this project is focused on helping participating hospitals identify and overcome barriers to establishing maternal milk supply and barriers to supporting breastfeeding in the NICU. Initiative to Improve Infant Nutrition and Care in NICUs
The Neonatal Subcommittee is responsible for initiating and overseeing the Increasing Breastfeeding and Human Milk Use in the NICU initiative.
The goal of the initiative, and its associated learning collaborative, is to increase the number of very low birth weight infants that will receive human milk, preferably their mother’s milk, as their primary source of nutrition to assist with their immune and gastrointestinal tract development. More specifically, this project is focused on helping participating hospitals identify and overcome barriers to establishing maternal milk supply and barriers to supporting breastfeeding in the NICU. Initiative to Improve Infant Nutrition and Care in NICUs
Currently there are nine Level III & six Level IV hospitals participating in the project, as well as two observing hospitals. Approximately 800 NICU beds are covered by the project.
The learning collaborative is designed to enable teams to share, test, and implement ideas for improving rates of human milk and breastfeeding among very low birth weight babies.
In particular, the collaborative working to increase the use of human milk and breastfeeding by focusing on components of a “NICU Breast Milk Feeding Bundle.” This bundle was developed through discussion through the participating hospitals throughout the state who have all been working to increase breastfeeding and the use of human milk in the NICU, and is informed by the extensive literature on breastmilk utilization in the NICU.
For more information on the initiative, visit the intervention page on this site.
Obstetrics Subcommittee Update
The Obstetrics Subcommittee continued working on its Induction of Labor (IOL) Quality Improvement (QI) project, to reduce failed indicated induction of labor and ultimately reduce the primary cesarean delivery rate in Texas.
August 2017
The Obstetrics Subcommittee continued working on its Induction of Labor (IOL) Quality Improvement (QI) project, to reduce failed indicated induction of labor and ultimately reduce the primary cesarean delivery rate in Texas.
Currently, four hospitals are participating in this QI project. Of these four, one hospital is the farthest along with completion of baseline data collection, and is possibly planning to implement the IOL protocol in fall 2017. The project has recently been launched in the remaining three hospitals.
The IOL QI project entails the adoption of a standardized IOL algorithm plus additional action steps as determined by the participating hospital.
Research Articles, Recommended by Our QI Chairs
We asked the chairs of our QI initiatives to share some of the research they've found valuable over the last few months. Here are the highlights:
We asked the chairs of our QI initiatives to share some of the research they've found valuable over the last few months. Here are the highlights:
From Dr. Nancy Hurst, Co-Chair of the Neonatal Subcommittee:
From Clinics in Perinatology: "Preterm Human Milk Macronutrient and Energy Composition: A Systematic Review and Meta-Analysis"
From Breastfeeding Medicine: "Barriers to Human Milk Feeding at Discharge of Very-Low-Birth-Weight Infants: Maternal Goal Setting as a Key Social Factor"
From the Journal of Perinatology: "Buccal administration of human colostrum: impact on the oral microbiota of premature infants"
From Dr. Christina Davidson, Co-Chair of the Obstetrics Subcommittee:
From Obstetrics and Gynecology: "Mechanical and Pharmacologic Methods of
Labor Induction: A Randomized Controlled Trial"
From ACOG Committee Opinion: "Management of Suboptimally Dated Pregnancies"
From June Hanke, Co-Chair of the Community Health Subcommittee:
From Obstetrics & Gynecology: "Maternal Cardiovascular Mortality in Illinois, 2002-2011"
From Maternal Child Health Journal: "Views of Women and Clinicians on Postpartum Preparation and Recovery"
From Janet Jones, Co-Chair of the Community Health Subcommittee:
From Pediatric Research: "The impact of intrauterine and extrauterine weight gain in premature infants on later body composition"
From Early Human Development: "A new type of swaddling clothing improved development of preterm infants in neonatal intensive care units"
From Dr. Catherine Eppes, Co-Chair of the Data Subcommittee:
From the Society for Maternal-Fetal Medicine: "Special Report: Current approaches to measuring quality of care in obstetrics"
From the Society for Maternal-Fetal Medicine: "The development and implementation of checklists in obstetrics"
From the American Journal of Obstetrics & Gynecology: "Reduction of severe maternal morbidity from hemorrhage using a state perinatal quality collaborative"
From the American Journal of Obstetrics & Gynecology: "Early standardized treatment of critical blood pressure elevations is associated with a reduction in eclampsia and severe maternal morbidity"
Maternal & Infant Health MMWRs
Differences in breastfeeding rates for black and white infants persist across the country, with serious health impacts. This and other recent CDC MMWRs related to maternal and infant health can be found here.
The Morbidity and Mortality Weekly Report (MMWR) is prepared by the Centers for Disease Control and Prevention (CDC). Published MMWRs aim to include “timely, reliable, authoritative, accurate, objective and useful public health information and recommendations.”
Below are selections from recent MMWRs that may be relevant to our TCHMB readers and collaborators, including “Racial and Geographic Differences in Breastfeeding – United States, 2011-2015.”
From Sept. 15, 2017 MMWR:
From Sept. 1, 2017 MMWR:
From August 25, 2017 MMWR:
"CDC Grand Rounds: Newborn Screening for Hearing Loss and Critical Congenital Heart Disease"
From August 11, 2017 MMWR:
From July 28, 2017 MMWR:
"CDC Grand Rounds: Addressing Health Disparities in Early Childhood"
From July 21, 2017 MMWR:
From July 14, 2017 MMWR:
“Racial and Geographic Differences in Breastfeeding – United States, 2011-2015”
From June 23, 2017 MMWR:
From June 16, 2017 MMWR:
From April 28, 2017 MMWR:
“Trends in Repeat Births and Use of Postpartum Contraception Among Teens – United States, 2004-2015”
From April 14, 2017 MMWR:
From April 7, 2017 MMWR:
Maternal & Infant Health News
From new state legislation for postpartum depression screenings to a look at what spiking maternal mortality rates mean for Texas, here's a list of all the biggest maternal and infant health news stories around Texas and the nation.
When two reports released in 2016 indicated that Texas mothers were dying at a rate higher than that of any developed nation, the state was shocked. Now, a number of hopeful solutions are in the works, from new legislation that aims to increase the number of women screened for postpartum depression to the creation of a new perinatal health center in Houston.
Nationwide, the maternal mortality rate remains troubling, and reporting projects from ProPublica and Vox take a closer look at what can be done. Meanwhile, the Zika virus continues to concern health care providers, though several vaccines are in the works, and NPR takes a look at breast-feeding norms from around the world.
Texas:
Washington Post - August 28, 2017
"The hurricane came, and these newborns refused to wait out the storm"
Large swaths of South Texas ground to a halt as Harvey dumped dozens of inches of rain on everything in its path. Some schools are closed until next month. Thousands of flights were canceled. Travel was stalled for anyone without a functioning boat. But some things could not wait.
Texas Tribune - August 16, 2017
"Gov. Abbott signs bill giving Texas maternal mortality task force more time"
After the close of the Texas Legislature's special session, Gov. Abbott signed a bill that will allow the state's Task Force on Maternal Mortality and Morbidity to continue its work until 2023. In a new release the governor said that he was "committed to doing everything we can to combat the maternal mortality rate in this state."
STAT News - August 9, 2017
"After her own complicated delivery, lawmaker aims to address Texas’s alarming maternal death rate"
In July, Thierry sponsored HB 11, colloquially called the “Texas Moms Matter Act,” which gives a state task force more time to collect data and study the causes of childbirth-related deaths.
Houston Press – July 17, 2017
“Despite Demand, Few Texas Women on Medicaid Are Able to Access IUDs”
In 2016, the Texas Health and Human Services Commission amended the state’s Medicaid rules, allowing hospitals to be reimbursed for offering new mothers on Medicaid access to Long-Acting Reversible Contraceptives (LARCs). But few hospitals have taken advantage of the rule change. One that has? Houston’s LBJ Hospital.
KUT – June 20, 2017
“Low-Income Moms Will Get Screened for Postpartum Depression During Baby Checkups”
In June, Governor Greg Abbott signed House Bill 2466, which increases screenings for postpartum depression among low-income Texas women. Under the law, which goes into effect in September, mothers covered by Medicaid or CHIP will be screened for PPD when they take their infants in for well-check appointments.
TMC News – June 6, 2017
“Maternal Mortality Rate in Texas”
Several independent reports showed Texas’s maternal mortality rates leading the developed world, capturing the state’s attention in 2016. Now researchers and health care professionals are working to better understand the data that supported those reports and to find a way forward.
Houston Chronicle – May 17, 2017
“New center takes aim at high-risk pregnancies, maternal mortality”
This May, two grants totaling about $1.7 million were awarded to create the March of Dimes Perinatal Safety Center, a collaboration between the University of Texas Health Science Center at Houston and Children’s Memorial Hermann Hospital. The new center will concentrate on developing a blueprint to improve infant and maternal mortality rates that can be implemented at hospitals nationwide.
Nation:
ProPublica – August 31, 2017
An extensive project by ProPublica, “Lost Mothers” aims to profile the estimated 700 to 900 women who died from pregnancy-related causes in the U.S. in 2016. 120 women have been identified by the team; full profiles of 16 are available to read online.
The Atlantic -- August 16, 2017
"At Last, a Big, Successful Trial of Probiotics"
An Indian study that involved more than 4,500 newborn babies found that providing the newborns with a synbiotic lowered their chance of developing sepsis by 40 percent.
The Atlantic – July 12, 2017
“Growing Cheaper Embryos for IVF Inside the Vagina”
A new incubator, called INVOcell, may provide a cheaper, more accessible alternative to traditional in-vitro fertilization, says Dallas-based reproductive endocrinologist Kevin Doody. But will it catch on?
The Atlantic – July 6, 2017
“The Case for Testing Zika Vaccines on Pregnant Women”
Though pregnant women are almost never included in medical research such as vaccine testing, a group of medical ethicists argue that pregnant women should be part of any clinical trials for Zika vaccines. After all, they’re the ones with the most at risk.
NPR – June 26, 2017
“Secrets of Breast-feeding from Global Moms in the Know”
Anthropologists like Brooke Scelza once wondered why American women seemed to struggle more than most with breast-feeding. Did women from other cultures have better breast-feeding instincts? Scelza traveled to Namibia to find out.
New York Times – June 12, 2017
“Practicing What I Preached About Breast-Feeding”
Pediatricians regularly recommend new mothers follow the AAP’s guidelines: exclusive breast-feeding for a baby’s first six months, and continued breast-feeding for a year. But how easy are those guidelines to follow? Dr. Perri Klass, a practicing pediatrician, committed to following those recommendations for her own third child, and shares the experience in the Times.
Vox – June 29, 2017
“California decided it was tired of women bleeding to death in childbirth”
Maternal mortality rates in the U.S. have been climbing, especially in Texas, where the rates are some of the highest in the developed world. But in California, the maternal mortality rate is a third of the U.S. average, largely due to the work of the California Maternal Quality Care Collaborative (CMQCC).